REDUCTION OF URIC ACID DEPOSITION
ONGOING URIC ACID DEPOSITION
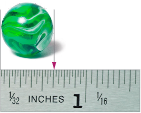
- 0-4.0 mg/dL1,2
- 4.1-5.9 mg/dL1,10
- >6.0 mg/dL5-7
0-4.0 mg/dL1,2
Potential to
- Resolve tophi faster
- Expedite the reduction of
uric acid burden
- 0-4.0 mg/dL1,2
- 4.1-5.9 mg/dL1,10
- >6.0 mg/dL5-7
4.1-5.9 mg/dL1,10
- Slow resolution of tophi
- Decrease flare frequency
- 0-4.0 mg/dL1,2
- 4.1-5.9 mg/dL1,10
- >6.0 mg/dL5-7
>6.0 mg/dL5-7
- Uric acid continues to deposit in the joints and tissues, including organs
- Flares can increase in frequency